

Neurodegenerative diseases represent a group of debilitating conditions characterised by the progressive degeneration and dysfunction of neurons in the central nervous system. These disorders, including Parkinson’s disease, Alzheimer’s disease, Huntington’s disease, and Amyotrophic Lateral Sclerosis (ALS), impose immense physical, emotional, and cognitive burdens on affected individuals.
These diseases can lead to devastating consequences such as the loss of motor control, impaired memory and cognition, muscle weakness or paralysis, mood disturbances, and eventually a significant decrease in quality of life.
Additionally, there is often an unmet need for adequate medical treatment options that can slow disease progression or alleviate symptoms effectively. Neurodegenerative diseases not only compromise the autonomy of patients but also place a strain on caregivers and healthcare systems due to prolonged care requirements.
A variety of causes and risk factors have been identified that contribute to the development of these debilitating conditions.
Let us take a look at some of the common kinds of ailments.
Alzheimer’s disease is a progressive neurodegenerative disorder that primarily affects older adults, causing memory loss, cognitive decline, and behavioural changes. It is the most prevalent cause of dementia among older adults, gradually impairing an individual’s ability to perform daily tasks, communicate effectively, and maintain relationships.

Causes: The exact cause of Alzheimer’s disease is not fully understood, but it is thought to involve a combination of genetic, environmental, and lifestyle factors. Age is the biggest risk factor, with the likelihood of developing the disease increasing significantly after the age of 65. Family history, genetics, and certain medical conditions may also contribute to the risk.
Diagnosis and Treatment: The diagnosis of Alzheimer’s disease involves a comprehensive assessment of medical history, cognitive abilities, and physical and neurological examinations. Although there is currently no cure, an early diagnosis enables effective symptom management and interventions to enhance the individual’s quality of life. Treatment options may include medications to address cognitive symptoms and behavioural changes, in addition to the invaluable support provided by healthcare professionals, caregivers, and support groups.
Parkinson’s disease is a chronic and progressive neurodegenerative disorder that primarily affects movement and can also lead to a range of other physical and cognitive symptoms.
It is characterised by the gradual loss of dopamine-producing cells in the brain, which affects the brain’s ability to control movement.

Causes and Risk Factors: While the exact cause of Parkinson’s disease is not fully understood, it is believed to involve a combination of genetic, environmental, and age-related factors. A history of family members with the disease can slightly increase the risk.
Diagnosis and Treatment: Diagnosing Parkinson’s disease involves clinical evaluation, medical history, and neurological exams. There are no specific tests to definitively diagnose the disease, but brain imaging can sometimes aid in ruling out other conditions. Treatment aims to manage symptoms, and medications that increase dopamine levels or mimic its effects are often prescribed. Physical therapy, speech therapy, and lifestyle modifications can also be beneficial.
Huntington’s disease is a hereditary, progressive neurodegenerative disorder that affects both physical and cognitive functions. It is caused by a genetic mutation that leads to the gradual degeneration of nerve cells in certain areas of the brain. The disease typically manifests in mid-adulthood, although it can appear earlier or later in life.
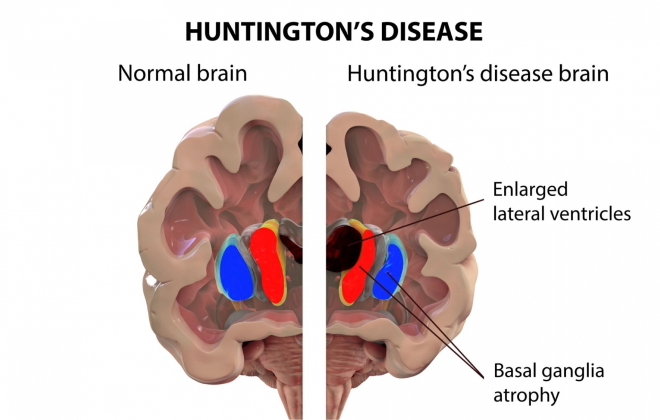
Causes and Risk Factors: Huntington’s disease is caused by a mutation in the HTT gene, which leads to the production of a mutant protein called Huntingtin. This mutant protein accumulates in neurons and interferes with their normal function, eventually causing cell death.
A child of a parent with the mutated gene has a 50% chance of inheriting the mutation associated with Huntington’s disease. If a person inherits the mutation, they will eventually develop the disease, typically between their 30s and 50s.
Diagnosis: Diagnosing Huntington’s disease involves conducting genetic testing to identify the presence of the mutated HTT gene. In certain instances, clinical symptoms and family history can also provide valuable information for diagnosis. It is highly recommended for individuals considering testing to seek genetic counselling, as the results can have significant implications for both the individual and their family.
Management and Treatment: Currently, there is no cure for Huntington’s disease. However, the primary goal of treatment is to effectively manage symptoms and enhance the overall quality of life. Medications play a crucial role in controlling both movement and mood-related symptoms.
Additionally, physical therapy, occupational therapy, speech therapy, and psychological support are vital components of care that should not be overlooked. These various approaches work together to provide comprehensive support and improve the well-being of individuals with Huntington’s disease.
Amyotrophic Lateral Sclerosis (ALS), also known as Lou Gehrig’s disease, is a progressive neurodegenerative disorder that primarily affects motor neurons, the nerve cells responsible for controlling voluntary muscle movement. ALS results in the gradual degeneration and loss of these motor neurons, leading to muscle weakness, paralysis, and ultimately difficulty in speaking, swallowing, and breathing.

Causes and Risk Factors: The precise cause of ALS is not completely understood, but it is believed that a mix of genetic and environmental factors plays a role. Mutations in specific genes, like the C9orf72 gene, are linked to familial ALS.
Diagnosis: Diagnosing ALS requires a thorough medical history, a neurological examination, and electromyography (EMG) to assess nerve and muscle function. It is also crucial to rule out other conditions that may have similar symptoms. It’s important to note that there isn’t a single definitive test for ALS.
Management and Treatment: There is currently no cure for ALS, but various interventions aim to manage symptoms, slow disease progression, and improve quality of life. Treatment may involve:
Multiple sclerosis (MS) is a chronic autoimmune disorder that affects the central nervous system, including the brain and spinal cord. It disrupts the communication between nerve cells, causing a wide range of unpredictable symptoms that can differ greatly from person to person. In multiple sclerosis, the immune system mistakenly attacks the protective covering of nerve fibres, leading to disruptions in neural signalling.
The most common form is relapsing-remitting multiple sclerosis (RRMS), where individuals experience periods of flare-ups (relapses or exacerbations) followed by periods of partial or complete recovery (remissions). Over time, some individuals with RRMS may transition to secondary progressive multiple sclerosis (SPMS), where symptoms gradually worsen without distinct relapses and remissions.

The symptoms of multiple sclerosis are diverse and can affect virtually any part of the body. Common symptoms include fatigue, numbness or tingling, muscle weakness, difficulty with coordination and balance, vision problems, and cognitive changes.
In primary progressive multiple sclerosis, symptoms worsen gradually from the onset without distinct relapses or remissions. A relapse or exacerbation is marked by the sudden worsening of existing symptoms or the appearance of new symptoms. These episodes can be mild or severe and vary in duration.
Causes and Risk Factors: The precise cause of multiple sclerosis is not yet fully understood, but it is believed to result from a combination of genetic susceptibility and environmental triggers. These triggers can include infections or exposure to specific toxins. Interestingly, multiple sclerosis tends to be more prevalent in certain geographical regions, which suggests that environmental factors may play a significant role in its development.
Diagnosis: Diagnosing multiple sclerosis requires a combination of analysis of medical history, neurological examination, and imaging studies such as MRI to identify any lesions in the central nervous system. Additionally, a lumbar puncture, also known as a spinal tap, can be performed to detect any abnormalities in the cerebrospinal fluid.
Management and Treatment: Although there is currently no cure for multiple sclerosis, the primary goal of treatment is to effectively manage symptoms, prevent relapses, and slow down the progression of the disease. To achieve this, a combination of medications, physical therapy, occupational therapy, and lifestyle adjustments are crucial in effectively managing the condition.
Living with a neurodegenerative disease is not easy. One may undergo numerous challenges. Here are some tips to navigate through this difficult phase of life.
Neurodegenerative diseases like Alzheimer’s, Parkinson’s, and Huntington’s are a significant global health burden, affecting individuals and families. Though there is still much to learn about their early diagnosis and prevention, there has been significant progress in understanding these diseases and hence managing them.
Nevertheless, continued research is essential to develop effective treatments and to uncover early diagnostic markers and preventive measures.
Sources:
Spread the love, follow us on our social media channels