


Joint pain and stiffness are common complaints, often broadly termed “arthritis.” However, this encompasses diverse conditions, notably rheumatoid arthritis (RA) and osteoarthritis (OA). While both affect joints, their underlying mechanisms, symptoms, progression, and treatments differ fundamentally. Misdiagnosis can delay effective management, significantly impacting quality of life. Understanding these distinctions is vital for anyone experiencing joint issues, guiding them towards appropriate medical advice and the correct path to joint health.
Let’s decode the difference between the two in this article.
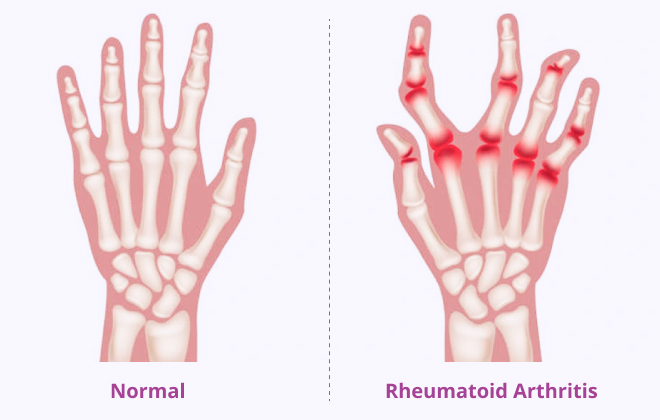
Rheumatoid arthritis is a chronic, systemic autoimmune disease. Here, the body’s immune system mistakenly attacks its own tissues, primarily the synovium – the joint lining.
This causes inflammation, pain, swelling, stiffness, and potential severe joint damage. As a systemic disease, RA can also affect organs beyond joints, including the heart, lungs, eyes, and blood vessels.
RA’s exact cause is unclear, but it involves genetic predisposition and environmental triggers.
Specific genetic markers, especially HLA (human leukocyte antigen) gene variants, increase RA risk. However, genetics alone don’t guarantee the disease.
In RA, the immune system fails to distinguish healthy tissue from invaders, producing antibodies (e.g., rheumatoid factor, anti-CCP) that attack the body’s components. This leads to chronic inflammation.
Factors thought to initiate RA in susceptible individuals include:
RA symptoms often develop gradually over weeks or months, distinct from other arthritis forms.
Firm lumps near joints.
A serious complication causing red, painful eyes, blurred vision, and light sensitivity, requiring urgent medical attention.
Can affect lungs, heart, and nerves, or cause anaemia.
You can read our article Rheumatoid Arthritis: Causes, Symptoms, and Cutting-Edge Treatments for a detailed understanding of this disease.
Osteoarthritis, or “wear and tear” arthritis, is the most common arthritis. It’s a degenerative condition from the breakdown of cartilage – the smooth tissue cushioning bone ends in joints. As cartilage wears, bones can rub directly, causing pain, stiffness, and reduced movement. OA is generally localised to affected joints, without systemic inflammation.
OA is multifactorial, arising from mechanical stress and biological processes.
OA symptoms typically develop slowly over many years, often localised to the affected joint(s).
Here’s a quick snapshot of what are the differences between osteoarthritis and rheumatoid arthritis.
| Rheumatoid Arthritis (RA) | Osteoarthritis (OA) | |
|---|---|---|
| Nature | Autoimmune, inflammatory, systemic | Degenerative, “wear and tear” |
| Cause | Immune system attacks synovium | Cartilage breakdown |
| Affected Joints | Symmetrical; often small joints (hands/feet) first | Asymmetrical; large weight-bearing joints, finger ends |
| Morning Stiffness | >30 minutes (often hours); improves with activity | <30 minutes; improves with movement after rest |
| Pain Pattern | Worse with rest/inactivity; better with movement | Worse with activity/weight-bearing; better with rest |
| Systemic Symptoms | Common (fatigue, fever, organ involvement) | Rare; localised to joints |
| Joint Appearance | Warm, swollen, tender, often red | Less warmth/redness; swelling from bone spurs/mild fluid |
| Onset Age | Typically between 30-50 years of age | Usually >50 years of age |
| Progression | Flares/remission; potential rapid joint damage | Slow, gradual |

Living with either RA or OA requires ongoing management. While neither is curable, modern treatments significantly improve outcomes. For RA, early, aggressive DMARD (Disease-Modifying Anti-Rheumatic Drugs) treatment has transformed the outlook, reducing joint destruction.
For OA, focusing on lifestyle, pain management, and surgical options like joint replacement can provide substantial relief and improved mobility. Consistent communication with healthcare professionals, treatment adherence, and active rehabilitation are essential for long-term well-being.
Rheumatoid arthritis and osteoarthritis, though both affect joints, are fundamentally distinct. RA is a systemic autoimmune inflammatory condition, typically affecting joints symmetrically with widespread symptoms. OA is a degenerative process, primarily cartilage breakdown, often affecting larger, weight-bearing joints asymmetrically with localised symptoms. Accurate differentiation via clinical assessment, blood tests, and imaging is crucial. This guides modern management: RA treatments focus on immune modulation to prevent destruction, while OA treatments prioritise pain relief, functional preservation, and, when necessary, joint replacement. Understanding these differences empowers patients and healthcare providers to ensure optimal care, promoting improved joint health and quality of life.

Dr Adrian Mark Masnammany
Consultant Physician & Rheumatologist
Sources:
Spread the love, follow us on our social media channels