


Minimally invasive spine surgery involves using small incisions and specialised instruments to treat various spinal disorders. The surgery can be performed to treat a variety of spine conditions such as herniated discs, spinal stenosis, scoliosis, spondylolisthesis, spinal tumours, numbness, weakness, or disability in some cases. It aims to reduce damage to the surrounding muscles and tissues.
Minimally invasive spine surgery (MISS) offers an alternative to traditional open-spine surgery involving larger incisions and more tissue disruption. It can achieve similar or better results using smaller incisions and advanced technologies with less pain, blood loss, infection risk, hospital stay, and recovery time.
However, it is not suitable for everyone or every condition. It also requires skilled surgeons who are familiar with the techniques and technologies of MISS. Therefore, patients considering MISS should consult with their doctors about the benefits and risks of this procedure.
MISS can treat spinal conditions that cause back, neck, arm, or leg pain, a weakened feeling, or numbness in the legs.
Here are some of the common conditions that MISS can treat:

MISS uses small incisions and specialised instruments to treat some of these conditions without causing much damage to the surrounding tissues.
It can help improve your quality of life by reducing or eliminating your pain and other symptoms, improving your mobility and posture, and preventing further damage to your spine.
Different techniques and approaches exist for performing MISS – depending on the location and severity of the spinal problem.
Some of the common types of MISS are:
This technique involves inserting a small tube through a tiny incision in the skin and muscle, creating a tunnel to access the spine. The surgeon then uses small instruments and a microscope or an endoscope to perform the surgery through the tube. The tube also helps to keep the muscles and tissues away from the surgical area, reducing blood loss and inflammation. This technique is often used for decompression surgeries, such as discectomy or laminectomy.
This procedure entails making a tiny incision in the skin and inserting an endoscope, a narrow, bendable tube containing a little camera and light. The endoscope allows the surgeon to see the inside of the spine on a monitor and guide the surgical instruments. The endoscope also helps to remove any damaged tissue or bone fragments from the spine. This procedure is often used for herniated disc repair or spinal fusion.
This method requires a small incision in the side of the body, close to the waist or lower back, to access the spine from the side. The surgeon then uses special instruments and retractors to move the organs and blood vessels away from the spine, creating a clear path to perform the surgery. This method is often used for spinal fusion or correcting spinal deformities.
Your quality of life is affected by the significant choice of whether or not to have spine surgery and what kind of spine surgery to have.
In general, there are two primary spine surgery procedures:
Open surgery involves a long incision that allows the surgeon to see and access the spine more easily. By cutting through the skin and muscles, the surgeon can remove portions of bone or disc to decompress the nerves or spinal cord (decompression) or insert screws, rods, cages, or bone grafts to fuse two or more vertebrae (fusion). Open surgery can treat more complex spinal conditions that may not be amenable to MISS.
Both approaches have benefits and drawbacks, but the best option depends on several factors, such as your condition, medical history, personal preferences and most importantly, your doctor’s recommendation.
The choice between MISS and open surgery depends on several significant factors, such as:
MISS can offer several advantages over open surgery, such as:
However, MISS is not free from limitations and challenges. Some of them are:
MISS has been evolving rapidly in recent years, thanks to the development of new technologies and techniques that have improved the procedure’s safety, accuracy, and effectiveness. Some of the advancements in MISS are:
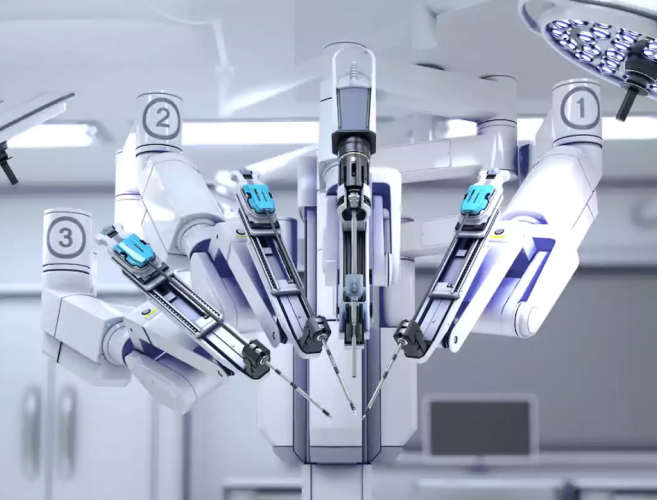
Robotic-assisted surgery is a method of performing spinal neurosurgery that uses a robotic device to assist the surgeon in guiding the surgical tools and implants through tiny openings in the skin. The robotic device, controlled by the surgeon through a console, has a robotic arm that can move with more accuracy, stability, and flexibility than the human hand. It can help the surgeon to perform delicate and complex procedures with less risk of damaging the surrounding tissues and nerves.
Robotic-assisted surgery can also lower the risk of radiation exposure for the patient, the surgeon, and the operating room staff by reducing the need for X-rays or fluoroscopy, which are imaging techniques that use radiation to show the body’s internal structures. Furthermore, robotic-assisted surgery can enhance the comfort and efficiency of the surgeon by improving the ergonomics of the surgical position and reducing the mental and physical fatigue that can result from prolonged and laborious operations.

Endoscopy has advanced significantly in recent years thanks to the development of new instruments, technologies, and approaches. Some of the advancements include:
As an advancement in spine surgery, MISS offers several benefits over traditional open-spine surgery, which uses larger incisions and may cause more tissue disruption. It can achieve similar or better results using smaller incisions and advanced technologies with less pain, blood loss, infection risk, hospital stay, and recovery time. Some of the advanced technologies that MISS uses are:
MISS is a promising option for patients with spine conditions seeking a less invasive and more effective treatment. By accurately navigating the spine, MISS can offer a better surgical experience and a faster recovery. MISS can also reduce open surgery’s potential complications and long-term effects on the spine.
Sources:
Spread the love, follow us on our social media channels