


Oral diseases are some of the most common noncommunicable diseases in Asia, according to the World Health Organization (WHO). They affect nearly half the population (45%) in their lifetime. Tooth decay, gum disease, oral cancer, and tooth loss are some of the most common oral diseases which are caused by a range of risk factors that can be changed, such as alcohol, tobacco, and sugar use, poor hygiene, and their social and economic causes.
Oral Surgery, a dentistry speciality, focuses on treating problems in the oral, maxillofacial, and facial regions. These problems can include diseases, injuries, and defects that affect the mouth, jaw, and face. A surgery can help in improving your oral health, and appearance. This includes a wide range of procedures – from simple tooth removal to complex facial reconstruction.
Oral surgeons are dentists with additional training and qualifications in oral surgery procedures. They are also trained to administer general anaesthesia, a requirement for oral surgeons in Malaysia and other Asian countries. Some oral surgeons may specialise in certain areas of oral surgery, such as cosmetic facial surgery, craniofacial surgery, microvascular surgery, or head and neck cancer surgery.
Oral surgery is a regulated dental speciality requiring advanced skills and knowledge. Oral surgeons in Malaysia need to follow the quality and safety standards laid out by government medical authorities and respective professional bodies.
Let’s take a look at a few common oral surgery procedures:

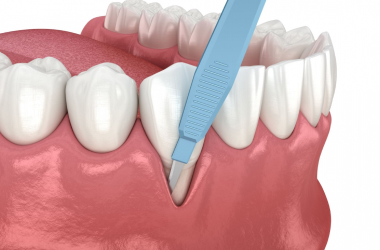
A dentist extracts a tooth that is damaged, decayed, infected, or impacted (wisdom tooth). The area of the tooth is numbed using local anaesthesia before the dentist removes the tooth. The recovery time depends on the number and location of the extracted teeth. The cost of tooth extraction in Malaysia can range from RM 50 to RM 500 per tooth.

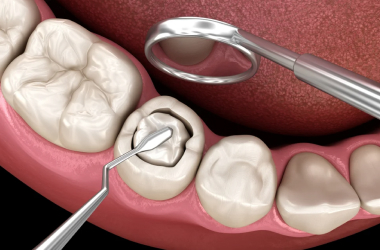
This surgery replaces missing dentition with prosthetic teeth attached to the jawbone. Dental implants can make your teeth work and look as they did before, preventing bone loss and the shifting of adjacent teeth. Dental implants usually require multiple dental appointments and may involve bone grafting, if there is insufficient bone.
The cost of dental implants in Malaysia varies depending on the type and number of implants. However, in general, it can range from RM 4000 to RM 10,000 per implant.

This surgical procedure adds bone tissue to areas with bone loss or deficiency, such as in the jawbone or around dental implants. Bone grafting can help increase the stability and success of dental implants and improve the shape and contour of the jaw. A dentist can use bones from another part of the body (autogenous), from a donor (allogenic), from an animal (xenogeneic), or from synthetic materials (alloplastic) to graft a tooth.
The cost of bone grafting in Malaysia depends on the source and amount of bone used, but it can be anywhere between RM 500 and RM 3000 per site.
This surgical procedure covers the roots of an exposed tooth with gum tissue from another part of the mouth or a donor. Gum grafting can help treat gum recession, which can cause tooth sensitivity, decay, and erosion. Grafting can also improve the appearance and health of the gums. To graft a gum, a dentist can use different techniques, such as free gingival grafting, connective tissue grafting, or pedicle grafting.
The cost of gum grafting in Malaysia depends on the type and extent of the graft; however, it can range between RM 800 and RM 2000 per tooth.

Jaw surgery involves the correction of the jaw, abnormalities or deformities of the upper and lower jaws, such as misalignment, overbite, underbite, or protrusion. The surgery can improve the function and appearance of the jaws, teeth, and facial profile and treat problems such as sleep apnoea, temporomandibular joint disorder (TMJ), and chronic pain. It is usually done under general anaesthesia and may involve cutting and moving the bones, placing plates and screws, or using orthodontic appliances. The recovery time for jaw surgery can take several weeks to several months and may require a liquid or soft diet.
The cost of surgery in Malaysia varies depending on the complexity and duration of the surgery, but it can range from RM 15,000 to RM 50,000.

This surgical procedure corrects congenital disabilities that affect the development of the palate (mouth’s roof) or the lip. Cleft lip and palate can cause problems such as feeding difficulties, speech impairment, ear infections, dental anomalies, and psychosocial issues. Cleft lip and palate repair can restore the normal function and appearance of the lip and palate, as well as improve the quality of life of the affected individuals. The repair may require multiple surgeries over several years, depending on the severity and extent of the defect.
The Malaysian government subsidises the cost of cleft lip and palate repair under the National Cleft Lip & Palate Programme. A few eligible patients are provided with free treatment at selected hospitals as well.

Facial trauma surgery is a surgical procedure for treating fractures or injuries to the facial bones or soft tissues, such as those resulting from accidents, violence, sports, or animal bites. Trauma surgery can help repair damaged structures such as the nose, cheekbones, eye sockets, jawbone, or skin. The surgery can also help restore the normal function and appearance of the face and prevent complications such as infection or nerve damage. It may involve techniques such as open reduction internal fixation (ORIF), external fixation (EF), or flap reconstruction.
The cost of facial trauma surgery in Malaysia depends on the type and severity of the injury, but in general, it ranges from RM 2000 to RM 20,000.

It is a surgical procedure that removes malignant tumours or lesions affecting the oral cavity or the surrounding structures, such as the lips, tongue, gums, floor of the mouth, palate, or throat. Oral cancer surgery can help treat the primary site of the cancer as well as prevent its spread to other parts of the body. Depending on the stage and type of oral cancer, Doctors may combine cancer surgery with additional therapies like radiation or chemotherapy. Oral cancer surgery may also involve Reconstructive surgery to improve the injured area’s look and functionality.
The cost of oral cancer surgery in Malaysia depends on the extent and location of the tumour and generally ranges from RM 5,000 to RM 50,000.

When the tissues in the back of the throat collapse during sleep, they block the airway causing obstructive sleep apnoea (OSA), more commonly known as sleep apnea. While some people with OSA can manage their condition with non-surgical methods, others with severe OSA may need surgery to remove or reposition the tissues that cause the obstruction.
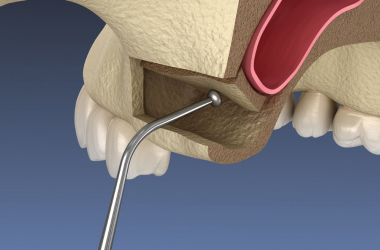
Adding bone to the upper jaw near the back molars is known as a sinus lift. This may be required when the maxillary sinus is too close to the upper jaw. A sinus lift involves lifting the sinus cavity’s membrane and placing bone graft material underneath it.
Gum infections and inflammations are both symptoms of gum disease, which may cause bone loss and tooth loss. To treat this condition, the oral surgeon may need to perform periodontal surgery. Periodontal surgery involves reshaping the gums or covering the exposed roots of the teeth.

Sometimes, teeth do not come out fully or into the mouth. These are called impacted teeth, which can cause problems such as pain, infection, damage to nearby teeth, or cysts. To remove impacted teeth, the oral surgeon makes a small cut in the gum and pulls out the tooth with a tool or a drill. If the surgery is to correct the position of the jaws, braces may be needed before and after the surgery to align the teeth properly.
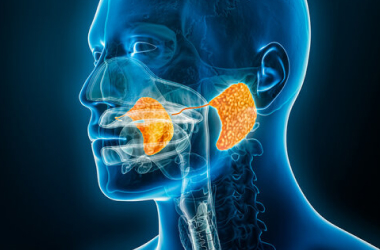
This is a condition where stones form in the salivary glands or ducts. They may restrict salivary flow and result in swelling, pain, dry mouth, or infection. Sialendoscopy is a minimally invasive treatment that uses a slim tube containing a camera and equipment to remove the stones from the salivary glands or ducts.

They are abnormal growths or lesions that can appear in the mouth or lips. Common causes of oral lumps and bumps are infections, inflammation, trauma, cysts, tumours, or cancer. The oral surgeon takes a tissue sample for a biopsy to diagnose oral lumps and bumps and examines the cells under a microscope. The treatment options for oral lumps and bumps depend on the cause and type of growth. They may include medication, laser therapy, cryotherapy (freezing), or surgery.

In this condition, your mouth is difficult to open or close due to spasms or stiffness of the muscles that control your jaw movement. Medication, muscle relaxants, physical therapy, massage, acupuncture, or surgery can treat lockjaw.

The third molar usually starts between 17 and 25 years old. It can cause problems such as pain, infection, crowding, or damage to adjacent teeth if it is impacted, misaligned, or decayed. A wisdom tooth is often removed by making a small incision in the gum and extracting the tooth with forceps or a drill.

This abnormal face enlargement is due to fluid accumulation, inflammation, infection, trauma, or allergy. It can cause pain, discomfort, difficulty breathing, or vision problems. Medication, ice packs, elevation, drainage, or surgery are the possible treatments for facial swelling.
The choice of surgeon is crucial to the success of oral surgery and subsequent recovery. Hence, choosing wisely is important. Some of the most useful things to look at are reputation, technologies used and services offered. Choose a clinic which uses the latest technology and includes the entire spectrum of oral and maxillofacial services – from root canal and implants to oral maxillofacial surgery options. Always check the credentials, especially their certification, and whether they are licensed to perform oral surgery procedures.
Oral surgery is not without risks. Even simple procedures such as tooth extractions can have serious complications. Besides the general risks of surgery (such as excessive bleeding, poor scarring, post-operative infection, and a bad reaction to anaesthesia), oral surgery can also have specific risks, especially for reconstructive surgery or facial trauma cases.
Some of these risks are:
Ensure to have a detailed discussion with your oral surgeon before undergoing any procedure. It is equally important to convey your medical history and allergies to your Doctor to avoid any untoward incident.
While your oral surgeon will give you detailed instructions on post-procedure care, here are some of the general precautions you should take at home.
Signs of infection are fever, chills, pus, foul-smelling discharge, or redness around the wound. Signs of excessive bleeding are soaking more than one gauze pad per hour or having blood in your saliva. Signs of severe pain are pain that does not improve with painkillers or pain that spreads to your ear, eye, or neck.
The recovery time after an oral surgery depends on the kind and complexity of the procedure, overall health, and the patient’s healing capacity. Your oral surgeon will tell you when you can return to work or school based on your recovery status. You may have to rest for a few days for minor procedures, such as tooth extractions, or a few weeks for major procedures, such as jaw surgery. You may also be advised to avoid strenuous activities like sports or heavy lifting until you are completely healed.
Sources:
Spread the love, follow us on our social media channels