


The importance of bones in living a healthy life is not unknown. They give us the freedom to move by supporting our bodies. But that’s not all! They also protect our internal organs, produce blood cells, and store and release fats and minerals.
However, bones are susceptible to conditions or injuries that affect various parts of the body. These problems, commonly known as orthopaedic problems, can cause pain, stiffness, swelling, deformity, or loss of function in the affected parts. Some orthopaedic problems are present at birth, while others develop over time due to trauma, infection, inflammation, degeneration, or cancer.
In this article, we take a look at some of the most common orthopaedic conditions and ways to prevent and treat them.
Our skeletal system consists of 206 bones which are attached to our muscles with the help of connective tissues. As we age, our joints become stiff, thus leading to various orthopaedic issues. Here are some of the most common orthopaedic conditions, which should be treated on time.
This is the most common type of arthritis, affecting mainly the knees, hips, spine, and hands. Over time, the bone-end cushioning cartilage deteriorates, causing friction and irritation between the bones.
Osteoarthritis can make daily activities challenging and cause pain, stiffness, and reduced movement. Older people are more susceptible to developing osteoarthritis, overweight people, those with a family history of arthritis, and those with joint injuries.


Immune system dysfunction causes rheumatoid arthritis. It attacks the joints and other organs, causing chronic inflammation. It affects the synovium, the tissue that covers the joints and produces synovial fluid to lubricate them.
Rheumatoid arthritis can cause pain, swelling, warmth, redness, and joint deformity, especially in the hands and feet. It can also impact the heart, blood vessels, lungs, eyes, skin, and other organs. Rheumatoid arthritis is more common in women than men and usually occurs between the ages of 30 and 50.
An excess of uric acid causes gout, a form of arthritis. Uric acid is an unwanted by-product that the kidneys usually remove. But when the blood has too much uric acid, it can form crystals that get stuck in the joints and cause sudden, severe attacks of pain, swelling, warmth, and redness.
Gout affects only one joint at a time, often the big toe. Alcohol consumption, dehydration, eating specific foods (like red meat and shellfish), taking certain medications (like diuretics), and having kidney issues can all contribute to gout.


This condition makes the bones lose mass or density, making them weak and easy to break. Osteoporosis can increase the chance of fractures or cracks in the bones, especially in the wrist, hip, and spine.
Osteoporosis can be caused by age, hormonal changes (especially in women after menopause), low calcium or vitamin D intake, inactivity, smoking, drinking, the use of certain medicines (such as steroids or anticonvulsants), or other conditions (such as hyperthyroidism or celiac disease).
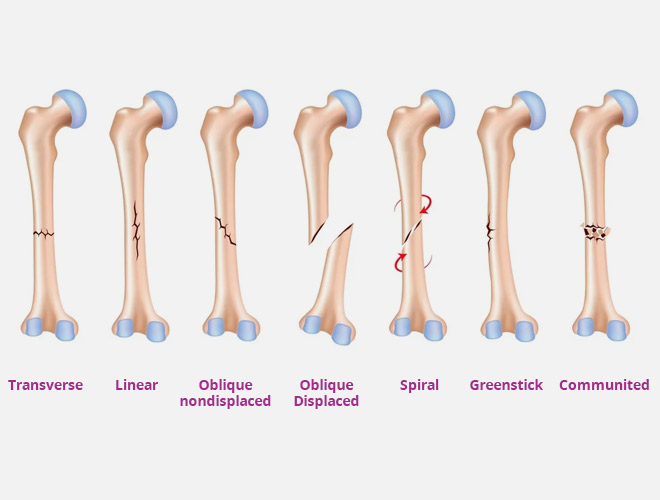
These are injuries that cause breaks or cracks in the bones from trauma (like falls or accidents), overuse (like repeated stress or strain), or disease (like osteoporosis or cancer). Fractures can cause pain, bruising, swelling, deformity, or loss of function in the affected bone or limb. Depending on certain factors, fractures can be of many types:

A condition in which the spine bends abnormally sideways. The spine can also twist or rotate around its axis. Scoliosis can cause back pain, uneven shoulders, hips, and waist, and a noticeable hump on one side of the ribs. Scoliosis can be present at birth (congenital) or have no known cause (idiopathic).
Idiopathic scoliosis usually starts in adolescence and affects girls more than boys. Scoliosis can be mild or severe, depending on how much the spine curves.
When the spine curves abnormally, it is known as kyphosis. The spine can look rounded or hunched. Kyphosis can cause back pain, stiffness, bad posture, breathing problems, or less mobility. It may be congenitally present at birth or develop later in life (acquired).
Aging, osteoporosis, spinal injuries, infections, tumours, and other conditions can all cause acquired kyphosis.


In this condition, the spinal column, spinal canal, and nerve roots get narrower. It can squeeze the spinal cord or nerve roots and cause pain, numbness, tingling, weakness, or cramping in the back, neck, arm, or leg.
Spinal stenosis can also make it hard to urinate or eat. Age, arthritis, disc degeneration, bone spurs, and spinal injuries are all potential causes of spinal stenosis.
This condition is where the cushion between the vertebrae, the soft gel-like material inside the spinal disc, sticks out or breaks via a crack in the disc’s cover. A herniated disc can squeeze the spinal cord or nerve roots and cause pain, numbness, tingling, weakness, and cramping in the back, neck, arm, and leg.
A herniated disc can also affect the bladder or bowels. Ageing, disc degeneration, trauma, lifting, twisting, or bending are all potential causes of herniated discs.


Carpal tunnel is a common condition in which the median nerve, which connects the forearm to the hand, gets inflamed or squeezed in the wrist’s carpal tunnel. Pain, numbness, burning, weakness of the thumb, the index, middle, and ring fingers, and tingling can be symptoms of carpal tunnel syndrome. Carpal tunnel syndrome can also affect gripping strength and hand coordination.
Repetitive hand movements, wrist injuries, arthritis, diabetes, pregnancy, or thyroid issues are all potential causes of carpal tunnel syndrome.
In this condition, the bursae, little sacs packed with fluid cushioning the joints, get inflamed or infected. Bursitis can cause pain, swelling, warmth, redness, or limited movement at the affected joint. Every body part is susceptible to bursitis.
However, the shoulder, elbow, hip, knee, and heel are the most common. Bursitis can be caused by overuse, injury, infection, arthritis, gout, diabetes, and other conditions.


Tendons are the fibrous cords that attach bones to muscles and transfer the contraction to the bones. Sometimes these tendons can get inflamed or irritated, leading to tendonitis. This can cause pain, swelling, warmth, redness, or limited movement at the affected tendon. All bodily tendons are susceptible to tendonitis; however, the shoulder (Rotator Cuff Tendonitis), elbow (Tennis or Golfer’s elbow), wrist (De Quervain’s Tenosynovitis), knee (Patellar Tendonitis), and heel (Achilles Tendonitis) are the most common.
Tendonitis can be caused by overuse, injury, infection, arthritis, gout, or diabetes.
These are injuries that happen when the ligaments, which are robust bands of connective tissue, stabilise bones at joints and limit their movement to prevent damage, stretch, or tear due to too much stress or twisting. Sprains can cause pain, bruising, swelling, instability, or limited movement at the affected joint. The ankle (inversion sprain), knee (medial collateral ligament sprain), and wrist (scapholunate ligament sprain) are the most common joints to get sprained, but any joint in the body can get sprained.
The severity of sprains can vary depending on how much the ligament is damaged. Sprains can be classified into different grades:

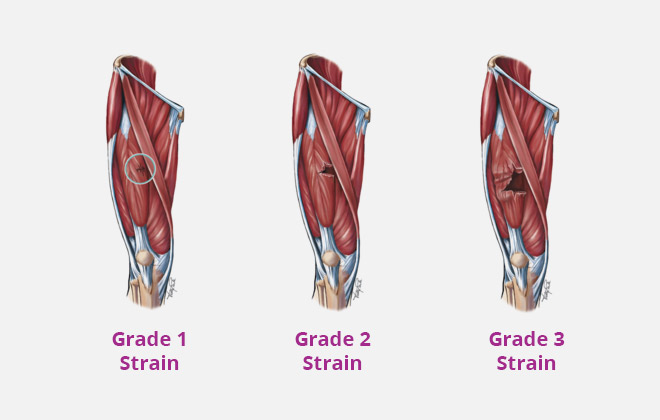
These injuries happen when the muscles or tendons, soft tissues that contract and relax to move the bones, get stretched or torn due to too much stress or overuse. It can cause pain, swelling, spasms, weakness, or limited movement in the affected muscle or tendon. The most common places for strains to occur in the body are the back (lumbar strain), neck (cervical strain), thigh (hamstring strain), calf (gastrocnemius strain), and groin (adductor strain).
Like sprains, strains are also classified into different levels based on how severe they are. The common grades of strain are:
The musculoskeletal system can get infected when bacteria, viruses, fungi, or parasites penetrate and multiply, resulting in inflammation, discomfort, swelling, redness, fever, or pus. Even though infections can affect any region of the musculoskeletal system, they are most frequently found in the joints (septic arthritis), bones (osteomyelitis), bursae (septic bursitis), tendons (septic tendinitis), and muscles (pyomyositis).
Injury, surgery, injections, foreign bodies, immunosuppression, diabetes, and poor hygiene are only a few of the causes of infections.


The aberrant cell growths known as tumours in the musculoskeletal system can be benign (non-cancerous) or malignant (cancerous). A tumour can cause pain, swelling, deformity, or loss of function in the affected body part. Tumours can occur in any part of the musculoskeletal system but are often found in the bones, soft tissues, and nerves.
Some examples of bone tumours are osteoma, osteosarcoma, chondroma, and chondrosarcoma. Some causes of tumours are radiation therapy, environmental exposure, genetic changes, and chronic inflammation.
Here are a few tips and recommendations to prevent common orthopaedic diseases:
Here are some of the things you can do: Use a chair that supports your lower back and lets your feet touch the ground.
Orthopaedic issues are common and can affect people of all ages. They can cause pain, swelling, stiffness, deformity, or loss of function in the musculoskeletal system. They can also affect quality of life, mental and physical health, independence, enjoyment, and self-esteem. However, there are ways to prevent and treat orthopaedic diseases and cope with their physical and psychological effects. By following some orthopaedic health tips and suggestions, one can maintain a strong musculoskeletal system and enjoy a better quality of life.
Sources:
Preventing Sports Injuries: Tips for Safe and Active Living
Spread the love, follow us on our social media channels