


The liver is one of the most important organs in our body with numerous metabolic, energy-storing, and waste-filtering functions. It aids in food digestion, production, and storage. It also helps to filter toxins from the bloodstream. It is an essential organ for the normal functioning of our body.
However, several illnesses and conditions can harm the liver and result in serious complications. This can harm our day-to-day life as well as lead to severe conditions that can be life-threatening as well.
In this article, we will explore some common types of liver-related diseases, their causes, symptoms, and treatments as well as share some tips on preventing them and maintaining a healthy liver.
Liver diseases can be classified into different categories based on their causes, such as:
Various virus strains can infect the liver and cause inflammation. These are the root cause of hepatitis A, B, C, D, and E. One may contract the hepatitis virus by touching contaminated surfaces or consuming contaminated food or water. They can also be contracted through blood transfusion and body fluid transfusion.
Some types of hepatitis can become chronic (long-term) and lead to cirrhosis (scarring), liver cancer, or liver failure. In Asia, hepatitis B and C are particularly prevalent, but screening or vaccination can prevent them.
In this kind of ailment, the immune system attacks healthy tissue liver and causes damage. Some examples are autoimmune hepatitis, primary biliary cholangitis (PBC), and primary sclerosing cholangitis (PSC). Although the precise reason for many of these illnesses is still unknown, environmental or genetic factors may play a role.
These are inherited conditions that affect the metabolism or storage of certain substances in the liver. Some examples are Wilson disease, hemochromatosis, alpha-1 antitrypsin deficiency, and cystic fibrosis. These disorders can cause the accumulation of toxic substances in the liver or other organs and lead to various complications.
These result from excessive alcohol consumption over a long period. Alcohol can inflame the liver and harm the cells, causing fatty deposits, fibrosis, cirrhosis, or cancer. The amount and duration of alcohol intake and other factors such as genetics, nutrition, and coexisting diseases can influence the severity and progression of alcohol-related liver illnesses.
Often known as NAFLD, this is caused due to the gathering of extra fat in the liver due to causes other than alcohol. NAFLD is becoming increasingly prevalent with the rise of diabetes and obesity.
NAFLD can be divided into two subtypes: non-alcoholic fatty liver (NAFL), which is usually benign and does not cause significant liver damage, and non-alcoholic steatohepatitis (NASH), which is a more severe form that involves inflammation and fibrosis and can progress to cirrhosis or cancer.
This is a malignant growth of abnormal cells in the liver. Hepatocellular carcinoma is the most typical liver cancer(HCC) originating from the liver cells. Other types include cholangiocarcinoma (bile duct cancer), angiosarcoma (blood vessel cancer), and metastatic cancer (cancer that spreads from other organs to the liver). Chronic viral hepatitis, cirrhosis, alcohol abuse, aflatoxin exposure, and genetic disorders can all contribute to liver cancer.
Liver diseases may not cause any symptoms in their early stages. However, some signs and symptoms may appear as the disease progresses and liver function deteriorates. These include:
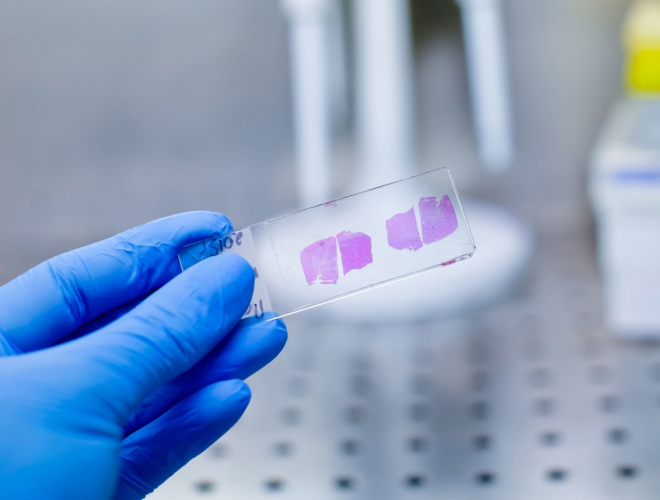
If you have symptoms or risk factors for liver disease, your healthcare provider may order some tests to evaluate your liver function and identify the cause of your condition. Some of the standard tests include:
Treatment for liver conditions depends on the type, cause, severity, and complications related to the ailment. Commonly, treatment may include:
Here are some ways to prevent liver diseases or reduce their progression:
If you have risk factors such as family history, obesity, diabetes, high cholesterol, or alcohol abuse, get regular check-ups and screenings for liver diseases.

The prognosis for people with liver diseases varies depending on the condition’s type, cause, severity, and complications. Some liver diseases can be cured with medications or surgery. Others can be controlled with supportive care and dietary adjustments. However, some liver diseases can progress to cirrhosis, liver failure, or liver cancer. These illnesses may necessitate a liver transplant and pose a hazard to life.
The best way to improve your outlook is to seek early diagnosis and treatment for any signs or symptoms of liver disease. You should also follow your healthcare provider’s recommendations on managing your liver and preventing further damage. Doing so can enhance your quality of life and avoid serious complications.
Among the vital functions, the liver performs many metabolic, energy-storing, and waste-filtering processes. It helps break down food, making and storing it until needed. Additionally, it helps with bloodstream toxicity filtration.
Therefore, taking good care of your liver and keeping it healthy is essential.

Taking care of your liver is of utmost importance. A healthy liver can enhance your overall health and well-being. It can help you digest food, produce energy, fight infections, regulate hormones, and more.
Taking care of your liver can also avoid the possibility of contracting major ailments such as cirrhosis, liver cancer, or liver failure.
Remember to consult your healthcare provider for any questions or concerns about your liver’s health. They can provide you with more information and advice on how to keep your liver healthy and functioning well.
Sources:
Spread the love, follow us on our social media channels