


Oncology is a vital field in medicine that focuses on the diagnosis, treatment, and prevention of cancer. Cancer is one of the leading causes of death worldwide accounting for nearly 1 in every 6 deaths in 2020. Cancer is the fourth leading cause of death in Malaysia, accounting for 12.6% of all deaths in government hospitals and 26.7% in private hospitals.
Advancements in the field of oncology give healthcare providers the necessary knowledge and skills to accurately diagnose different types of cancer. This helps in providing timely intervention and personalised treatment plans for each patient’s specific needs. Additionally, oncologists also recommend emotional support, and counselling services as well as help patients gain access to other healthcare teams involved in the patient’s care, guiding them throughout their cancer journey.
In addition to patient care, oncology research continually expands our understanding of this complex disease and contributes to the development of innovative therapies.
Cancer is a complex and diverse group of diseases that arise when abnormal cells in the body divide uncontrollably and invade surrounding tissues. There are over 100 different types of cancer, each with its unique characteristics, treatment options, and prognosis. Some common types of cancer include breast cancer, lung cancer, colorectal cancer, prostate cancer, and skin cancer.
According to a study on cancer survival in Malaysia published by the Ministry of Health, the 5 most common cancer cases in Malaysia are:
However, it is important to note that the prevalence of different types of cancers varies from one region to another and is affected by factors such as lifestyle choices, genetic predispositions, exposure to carcinogens, and access to healthcare services. Understanding the prevalence and characteristics of different types of cancers is crucial for early detection and effective management strategies.

Some of the most common risk factors for developing cancer include:
As individuals age, their risk of developing cancer increases due to accumulating changes in DNA that can lead to uncontrolled cell growth.
Individuals with a family history of certain types of cancer are more prone to developing the disease themselves. Lifestyle choices such as smoking tobacco, excessive alcohol consumption, and poor diet have been associated with an increased risk of various cancers. Exposure to environmental toxins such as asbestos or benzene and ionising radiation can also contribute to the development of cancer. Chronic inflammation resulting from conditions like autoimmune diseases or severe infections has been linked to an elevated risk as well.
Furthermore, certain infections caused by viruses such as human papillomavirus (HPV), hepatitis B and C viruses (HBV and HCV), and human immunodeficiency virus (HIV) can also increase the likelihood of developing specific cancers.
In Malaysia, one-third of deaths from cancers are caused by behavioural and dietary risks, low fruit and vegetable intake, lack of physical activities, high body mass index, and tobacco and alcohol use. In fact, tobacco has been identified as the leading cause of cancer in Malaysia causing 22% of total cancer deaths.
It is crucial for healthcare professionals to educate patients about these risk factors so they can make informed decisions regarding prevention strategies and go for regular screenings for early detection. According to WHO, 30-50% of cancer cases are preventable by avoiding risk factors and implementing prevention strategies.
Various kinds of diagnostic tests are used in the field of oncology to accurately detect and diagnose different types of cancer. These include imaging techniques such as X-rays, CT scans, MRI scans, and PET scans, which allow physicians to visualise tumours and assess their size and location.
Additionally, laboratory tests including blood tests, biopsies, and genetic testing which are commonly employed to analyse specific biomarkers or mutations that may indicate the presence of cancerous cells. Molecular tumour profiling is another increasingly important test that examines the genetic profile of a tumour to identify specific genetic alterations and guide personalised treatment options.
Liquid biopsy is a non-invasive test that analyses circulating tumour cells or fragments of DNA shed by a tumour into a person’s bloodstream. The combination of these diverse diagnostic tools enables oncologists to make accurate diagnoses, determine the stage of cancer, evaluate treatment responses, and customise individualised therapeutic approaches for patients with various malignancies.
When it comes to cancer, understanding and categorising its severity is crucial for determining the appropriate treatment and predicting outcomes. This information helps doctors formulate an effective treatment plan tailored to each patient’s unique situation.
Typically, cancer stages range from 0 to IV, with stage 0 being the earliest form that has not invaded nearby tissues and stage IV indicating that cancer has metastasized or spread to other organs or distant parts of the body.
Another essential aspect of assessing cancer is grading it based on its microscopic characteristics. Grading provides valuable insights into tumour aggressiveness and growth potential by evaluating factors such as abnormal cell shape, cell division rate, tissue differentiation, and mitotic activity. Typically graded between 1 (least aggressive) and 4 (most aggressive), a higher grade generally indicates a more challenging prognosis and a more aggressive treatment approach.
Consequently, comprehending both the stage and grade enables medical professionals to make informed decisions regarding patient management strategies in their fight against this formidable disease.
Treatment options such as surgery, chemotherapy, and radiation therapy continue to play a critical role in the management of various diseases. Surgery involves the physical removal of tumours or damaged tissue, aiming to eliminate the cancerous cells from the body. It is often considered the primary treatment for solid tumours that are localised and have not spread to other parts of the body.

Chemotherapy utilises powerful drugs that target rapidly dividing cells throughout the body, effectively killing cancer cells. It can be administered orally or intravenously and may cause side effects due to its non-selective nature.
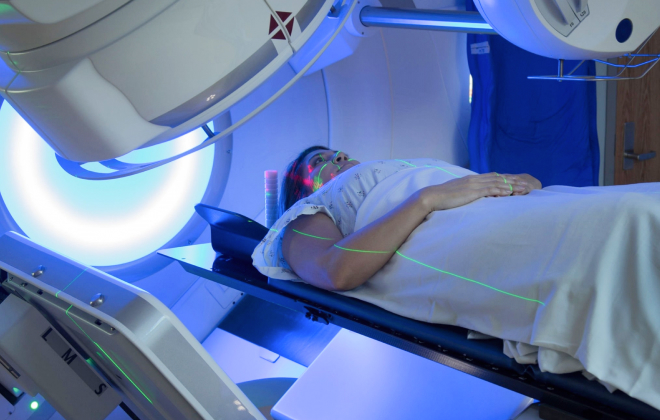
Radiation therapy delivers targeted doses of high-energy radiation to destroy cancer cells or shrink tumours. This localised treatment option may be used alone or in combination with surgery or chemotherapy, depending on the type of cancer.
While each treatment modality has its risks and benefits, they collectively offer hope in improving outcomes and extending a patient’s survival rate by eradicating or controlling disease progression through evidence-based interventions.
Targeted therapies and immunotherapy have revolutionised the field of cancer treatment, offering new hope for patients with various types of malignancies.
Targeted therapies are designed to identify specific molecular targets in cancer cells, thereby directly inhibiting their growth and survival.
These therapies involve the use of drugs that selectively bind to specific molecules, such as receptors or enzymes, that play a critical role in tumour development and progression.
By targeting these molecules with precision, targeted therapies aim to disrupt the signalling pathways necessary for tumour growth while sparing normal cells from damage.
Immunotherapy, on the other hand, harnesses the power of the immune system to recognise and destroy cancer cells. This approach includes a range of strategies designed to boost the immune response against tumours, such as immune checkpoint inhibitors and chimeric antigen receptor (CAR) T-cell therapy.
Immune checkpoint inhibitors block proteins that prevent T-cells from recognizing and attacking cancer cells, while the patient’s own T-cells are modified through CAR-T cell therapy to to express receptors that can recognize specific antigens on cancer cells.
Both targeted therapies and immunotherapies have shown remarkable success in clinical trials for different cancers, leading to improved patient outcomes and increased survival rates.
A multidisciplinary approach plays a crucial role in oncology care to ensure the best outcomes for patients. With cancer being a complex and multifaceted disease, addressing it requires expertise from various medical fields such as surgery, radiation oncology, medical oncology, pathology, and radiology. The collaborative effort of different specialists allows for comprehensive evaluation and treatment planning tailored to each patient’s unique circumstances.
By having a multidisciplinary team involved in cancer care, there is an increased opportunity for accurate diagnosis, timely intervention, and improved treatment decision-making. Such an approach also facilitates the management of potential side effects and complications associated with cancer treatments.
The importance of a multidisciplinary approach in oncology care cannot be overstated as it ensures comprehensive care that addresses all aspects of the disease while prioritising patient well-being and positive treatment outcomes.
Clinical trials are crucial for cancer treatment advancement. They evaluate new therapies, such as drugs and immunotherapies, to determine their effectiveness and safety. These trials follow strict guidelines and protocols, helping researchers find the best treatment options for patients. They also allow for the testing of surgical techniques and the discovery of biomarkers that can predict treatment response.
By involving diverse groups of patients, clinical trials generate data that improve existing treatments and develop innovative approaches. They offer patients the opportunity to contribute to research and potentially access cutting-edge treatments.
A survivorship care plan is a complete plan that includes a patient’s cancer and treatment history and the future roadmap. Survivorship care plans are important in managing patients after cancer treatment. They provide a roadmap for both patients and healthcare providers to ensure coordinated and patient-centred care.
These plans address the physical, emotional, and psychosocial needs of cancer survivors by providing information on follow-up appointments, potential late effects of treatment, recommended screenings, and healthy lifestyle recommendations.
They facilitate effective communication among healthcare professionals and empower patients to actively engage in self-care strategies. Ultimately, survivorship care plans improve the quality of life for cancer survivors by giving them knowledge and tools for long-term disease management.
Emotional support and counselling play a critical role in the well-being of cancer patients and their families. A cancer diagnosis can be overwhelming, leading to feelings of fear, anxiety, and depression.

Emotional support and counselling not only foster emotional well-being but also aid in empowering individuals to actively participate in their own care journey amidst the challenges posed by cancer.
Palliative care in oncology is a specialised type of medicine that focuses on improving the quality of life for cancer patients, especially during their final stages. It involves addressing physical symptoms such as pain and difficulty breathing, as well as providing emotional support and counselling for both patients and their families.
The goal here is to effectively manage the symptoms, allowing patients to maintain their dignity and independence. Palliative care teams consist of various healthcare professionals, such as pain management experts, nurses, social workers, and spiritual advisors. They collaborate with the patient’s primary oncologist to create a personalised care plan that respects the patient’s values and preferences.
Cancer is a serious disease causing one in six deaths across the world. Several risk factors cause cancer and hence, it is important to have a detailed knowledge of them to take preventive measures.

The stage at which cancer is detected has a direct effect on prognosis. Hence early diagnosis can help a patient access treatment and defeat cancer altogether. Cancer is detected through a variety of ways including blood tests, biopsies, and genetic testing and others.
The most commonly used treatment options of cancer include surgery, radiation therapy, chemotherapy, immunotherapy, targeted therapies, and hormone therapy.
Apart from medical intervention, providing emotional and psychological support to cancer patients throughout their journey is of utmost importance. The treatment team along with a supportive friend and family group can make a world of difference to the quality of life of a cancer patient.
Sources:
Spread the love, follow us on our social media channels