


A darkening of facial skin can be a significant concern. This change is often due to “hyperpigmentation,” where excessive or uneven melanin production leads to darker patches. More than a cosmetic issue, facial hyperpigmentation can signal various underlying causes, from common sun exposure to hormonal shifts or medical conditions.
Understanding its types, triggers, diagnosis, and modern treatments is crucial for effective management and restoring an even complexion. This article explores these aspects in detail.
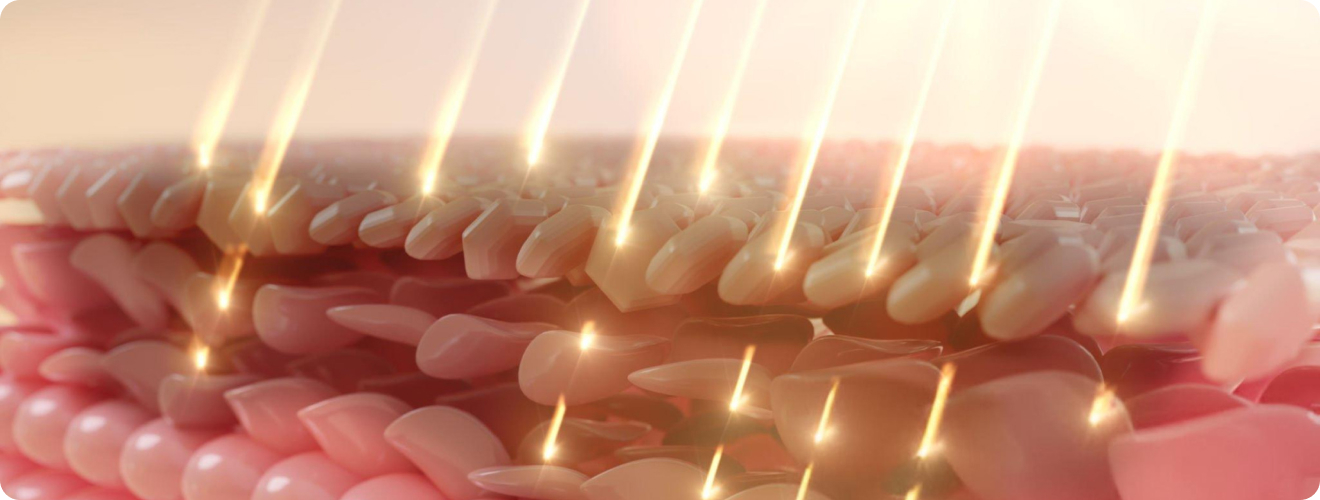
Facial skin darkening is primarily caused by hyperpigmentation, a broad term for skin patches darker than surrounding areas. This occurs when melanocytes, specialised skin cells, produce excessive melanin (the pigment for skin, hair, and eye colour) or when melanin is unevenly distributed. This overproduction or irregular clumping creates visible dark spots or patches. While “melanosis” refers to increased melanin, “hyperpigmentation” is the more common clinical term for its visible manifestation.
Facial hyperpigmentation stems from several distinct dermatological issues; identifying the specific type is key to effective treatment.
Several factors increase the risk of hyperpigmentation on the face:
Symptoms of facial hyperpigmentation vary based on the type of the pigmentation:
A dermatologist is best equipped to diagnose the specific type of facial hyperpigmentation.
What are the modern management techniques used for facial melanosis treatment? The procedures require patience, consistency, and often a dermatologist-guided combination approach.
Well, as goes the famous saying, “Prevention is better than cure”. So, let’s start with two primary prevention techniques:
These are the first-line options for melanosis skin treatment that inhibit melanin production or increase cell turnover.
Your doctor may suggest oral prescription medications such as Tranexamic Acid which are particularly effective for refractory melasma, inhibiting melanin production pathways. Requires careful medical supervision.
If the above lines of treatment do not work or the extent of hyperpigmentation is very high, your dermatologist may suggest certain procedures including:
Often the most effective approach, combining topical agents, potentially oral medication, and selected procedures, along with strict sun protection.
Addressing hormonal imbalances for melasma or effectively treating inflammatory skin conditions (e.g., acne) to prevent new PIH marks.

Managing facial hyperpigmentation is a long-term journey requiring patience and consistency. Results are gradual, taking months to become noticeable. Avoid self-treating with unverified products, as this can worsen pigmentation or cause permanent skin damage. The psychological impact should be acknowledged, seeking professional support if self-esteem is significantly affected. Regular dermatologist follow-ups are essential for monitoring progress, adjusting treatment, and long-term maintenance.
Facial skin darkening, or hyperpigmentation is a complex dermatological issue stemming from diverse causes, from sun exposure to hormonal and inflammatory processes. Accurately differentiating types like melasma, post-inflammatory hyperpigmentation, and solar lentigines is crucial for effective treatment. While UV radiation is a dominant risk factor, genetics, hormones, and skin trauma also play significant roles.
Modern management heavily relies on prevention, especially strict sun protection, complemented by tailored topical agents, oral medications, and targeted procedures. By understanding hyperpigmentation’s nuances and adhering to a comprehensive, professional-guided plan, individuals can significantly improve their skin tone, mitigate its impact, and regain confidence in their complexion.
Sources
Spread the love, follow us on our social media channels